Symptoms include left upper quadrant pain, left shoulder pain (Kehr sign), signs of peritonitis, and hemodynamic instability. Splenomegaly, age older than 40, or the presence of a neoplasm increases the risk of mortality from splenic rupture. Splenic rupture occurs in both adult and pediatric populations and should be suspected in patients with abdominal trauma or pre-existing conditions that increase the risk of splenomegaly.
Immediate resuscitation with fluids and blood products should be done. Focused assessment with sonography in trauma (FAST) examination and CT scan can be useful for diagnosis. Management of splenic rupture depends on the degree of injury but ranges from a conservative approach to angiographic embolectomy and emergent splenectomy.
The American Association for the Surgery of Trauma (AAST) has a spleen injury grading system based on imaging and intraoperative findings:
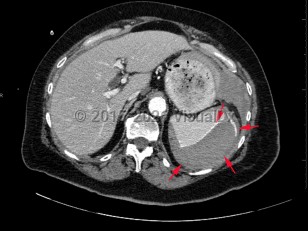
- Grade I: subcapsular hematoma < 10% of surface area; capsular tear; parenchymal laceration < 1 cm depth.
- Grade II: subcapsular hematoma 10%-50% of surface area; parenchymal laceration 1-3 cm in depth that does not involve a trabecular vessel.
- Grade III: subcapsular hematoma > 50% of surface area or expanding ruptured subcapsular or intraparenchymal hematoma; intraparenchymal hematoma > 5 cm in diameter or expanding; parenchymal laceration > 3 cm in depth or involving trabecular vessels.
- Grade IV: laceration involving segmental or hilar vessels producing major devascularization (> 25% of spleen). Grade V: completely shattered spleen; hilar vascular injury devascularizes spleen.