White piedra
Alerts and Notices
Important News & Links
Synopsis

White piedra is a relatively uncommon superficial fungal infection of the terminal hair shaft. It is caused by environmental, skin-colonizing fungi, primarily from the genus Trichosporon. Other implicated species include Acremonium, Brevibacterium, Candida, and Cladosporium. Coinfection with Corynebacterium species has been reported.
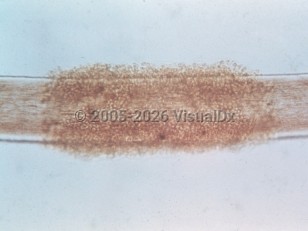
White piedra presents as soft, white, creamy white, or light brown nodular concretions along the terminal hair shaft. These concretions are distributed in an irregular manner and may coalesce to form tubular structures. They can be easily separated from the hair shaft. The infection is chronic and typically asymptomatic, although it does have the potential to cause hair breakage. The most common site affected by white piedra is the scalp, but pubic, axillary, and facial hair may also be affected. A variant presentation of white piedra of the scalp appears more like tinea capitis, with hyperkeratosis and alopecia with or without concretions along the hair shaft.
Patients affected by white piedra may be of any age, sex, and race / ethnicity, but it is most common in young female children. It is found in temperate and semitropical climates, including much of South America, Africa, Europe, the Middle East, Southeast Asia, India, and Japan. It has historically occurred infrequently in the United States, although an increasing number of documented cases have been occurring, including in the Northeastern and Southeastern United States.
Important risk factors for developing white piedra are long hair, use of a hair band or hair accessories, wet hair, living in an endemic area, humidity, poor personal hygiene, and hyperhidrosis. Spread through person-to-person contact is uncommon.
Immunocompromised patient considerations: Immunocompromised patients can develop severe, life-threatening sepsis from disseminated fungal infection from Trichosporon species (see Trichosporon sepsis). Cutaneous signs of dissemination include widespread purpuric papules and nodules with associated necrosis. This is seen most commonly in patients with neutropenia (including patients with hematologic malignancy and those undergoing chemotherapy), although it has been documented with other causes of immunosuppression, including AIDS. The vast majority of reported cases do not reference preceding white piedra.
White piedra presents as soft, white, creamy white, or light brown nodular concretions along the terminal hair shaft. These concretions are distributed in an irregular manner and may coalesce to form tubular structures. They can be easily separated from the hair shaft. The infection is chronic and typically asymptomatic, although it does have the potential to cause hair breakage. The most common site affected by white piedra is the scalp, but pubic, axillary, and facial hair may also be affected. A variant presentation of white piedra of the scalp appears more like tinea capitis, with hyperkeratosis and alopecia with or without concretions along the hair shaft.
Patients affected by white piedra may be of any age, sex, and race / ethnicity, but it is most common in young female children. It is found in temperate and semitropical climates, including much of South America, Africa, Europe, the Middle East, Southeast Asia, India, and Japan. It has historically occurred infrequently in the United States, although an increasing number of documented cases have been occurring, including in the Northeastern and Southeastern United States.
Important risk factors for developing white piedra are long hair, use of a hair band or hair accessories, wet hair, living in an endemic area, humidity, poor personal hygiene, and hyperhidrosis. Spread through person-to-person contact is uncommon.
Immunocompromised patient considerations: Immunocompromised patients can develop severe, life-threatening sepsis from disseminated fungal infection from Trichosporon species (see Trichosporon sepsis). Cutaneous signs of dissemination include widespread purpuric papules and nodules with associated necrosis. This is seen most commonly in patients with neutropenia (including patients with hematologic malignancy and those undergoing chemotherapy), although it has been documented with other causes of immunosuppression, including AIDS. The vast majority of reported cases do not reference preceding white piedra.
Codes
ICD10CM:
B36.2 – White piedra
SNOMEDCT:
35586003 – White piedra
B36.2 – White piedra
SNOMEDCT:
35586003 – White piedra
Look For
Subscription Required
Diagnostic Pearls
Subscription Required
Differential Diagnosis & Pitfalls

To perform a comparison, select diagnoses from the classic differential
Subscription Required
Best Tests
Subscription Required
Management Pearls
Subscription Required
Therapy
Subscription Required
References
Subscription Required
Last Reviewed:06/22/2024
Last Updated:07/07/2024
Last Updated:07/07/2024