Late congenital syphilis
See also in: Oral Mucosal LesionAlerts and Notices
Important News & Links
Synopsis

Syphilis crisis in the United States: Syphilis and congenital syphilis cases have been surging nationwide, with an 80% increase in total syphilis cases between 2018 and 2022. Serologic testing is the primary means of diagnosing, staging, and managing syphilis. Testing should be done for any sexually active patient in whom syphilis is suspected or who has new, unexplained symptoms. Prompt diagnosis and treatment of syphilis can prevent systemic complications, including ocular involvement and permanent blindness.
Congenital syphilis is a congenitally acquired infection with the bacterium Treponema pallidum. Although it is a relatively uncommon presentation, congenital syphilis can be a devastating diagnosis, and earlier diagnosis carries the potential for significant improvement to an affected individual's quality of life.
Transmission of T pallidum can occur in utero via the placenta after 4 months gestation, or through exposure to infectious vaginal lesions during delivery (perinatal syphilis). The subsequent signs and symptoms of congenital syphilis can be divided into two categories: (1) early congenital syphilis describes manifestations presenting before 2 years of age; (2) late congenital syphilis describes manifestations presenting after 2 years of age.
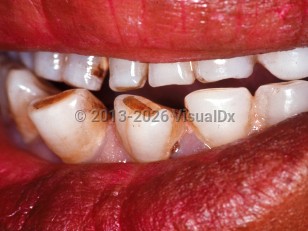
The symptoms of late congenital syphilis are analogous to tertiary syphilis in the adult. The signs and symptoms for both arise from either continued inflammatory processes against T pallidum antigens or attempts by the body to control the damage from infection in utero. Although late congenital syphilis is subclinical in 60% of cases, manifestations can occur into the early 20s and most commonly involve the bones, teeth, and nervous system. Hutchinson's triad, which is pathognomonic for late congenital syphilis, is defined by the presence of interstitial keratitis, Hutchinson incisors, and eighth nerve deafness.
Congenital syphilis is a congenitally acquired infection with the bacterium Treponema pallidum. Although it is a relatively uncommon presentation, congenital syphilis can be a devastating diagnosis, and earlier diagnosis carries the potential for significant improvement to an affected individual's quality of life.
Transmission of T pallidum can occur in utero via the placenta after 4 months gestation, or through exposure to infectious vaginal lesions during delivery (perinatal syphilis). The subsequent signs and symptoms of congenital syphilis can be divided into two categories: (1) early congenital syphilis describes manifestations presenting before 2 years of age; (2) late congenital syphilis describes manifestations presenting after 2 years of age.
The symptoms of late congenital syphilis are analogous to tertiary syphilis in the adult. The signs and symptoms for both arise from either continued inflammatory processes against T pallidum antigens or attempts by the body to control the damage from infection in utero. Although late congenital syphilis is subclinical in 60% of cases, manifestations can occur into the early 20s and most commonly involve the bones, teeth, and nervous system. Hutchinson's triad, which is pathognomonic for late congenital syphilis, is defined by the presence of interstitial keratitis, Hutchinson incisors, and eighth nerve deafness.
Codes
ICD10CM:
A50.7 – Late congenital syphilis, unspecified
SNOMEDCT:
82323002 – Late congenital syphilis (2 years OR more)
A50.7 – Late congenital syphilis, unspecified
SNOMEDCT:
82323002 – Late congenital syphilis (2 years OR more)
Look For
Subscription Required
Diagnostic Pearls
Subscription Required
Differential Diagnosis & Pitfalls

To perform a comparison, select diagnoses from the classic differential
Subscription Required
Best Tests
Subscription Required
Management Pearls
Subscription Required
Therapy
Subscription Required
References
Subscription Required
Last Reviewed:10/13/2021
Last Updated:04/03/2024
Last Updated:04/03/2024
Late congenital syphilis
See also in: Oral Mucosal Lesion