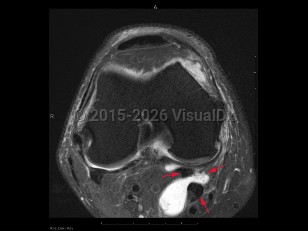
Causes / typical injury mechanism: A popliteal cyst, also known as a Baker cyst or a parameniscal cyst, is a synovial, fluid-filled swelling in the popliteal fossa behind the knee joint, located between the medial head of gastrocnemius and semimembranosus tendons. Anything that causes knee effusion can cause a popliteal cyst, including intraarticular pathology such as a
meniscal tear, inflammatory arthritis, or
rheumatoid arthritis. Typically, this cyst results from degeneration or weakening of the joint capsule, resulting in a one-way valve in which synovial fluid extravasates from the joint and forms a cyst posteriorly, which is typically the dependent position when the patient is lying supine. Uncommonly, the popliteal cyst can result in dissection, rupture, and compression to neurovascular structures with associated complications such as entrapped nerves,
compartment syndrome (rarely), and ischemia, requiring immediate care. More frequently, this is a self-limiting condition that resolves, relapses, and recurs without intervention.
Classic history and presentation: Popliteal cysts typically present as pain localized to the back of the knee with a sensation of stiffness and possible knee swelling. Weakness or claudication (secondary to neurovascular impingement) may be present.
Prevalence:
- Age – This can occur in all ages, but it is most common in older adults.
- Adults tend to have secondary Baker cysts.
- Pediatric popliteal cysts are usually primary, spontaneous, and self-resolving. They most commonly occur due to herniation of the posterior knee joint capsule synovium and are rarely due to injury. They are often asymptomatic, and they do not communicate with the joint space.
- Consider secondary pediatric Baker cysts if there is a history of juvenile idiopathic arthritis (JIA) or Lyme disease.
- Studies of asymptomatic knees have shown the prevalence of popliteal cysts to be anywhere from 4.7%-37%.They are often found incidentally on imaging.
- Sex / gender – No prevalence.
Risk factors:
Pathophysiology: Normally occurring bursa becomes distended, usually secondary and related to synovial fluid buildup due to joint pathology or injury, such as inflammatory arthritis, osteoarthritis, or a meniscus cartilage tear. These cysts may also arise spontaneously. In adults, the bursa has a communication with the posterior knee joint capsule at the level of the medial femoral condyle, allowing the fluid to flow into the bursa via a one-way valve. These cysts form posteriorly, as this is the dependent position where fluid would settle or collect when a patient is in the supine position (lying down).