- Patients with suspicion for acute appendicitis in the outpatient setting should be referred to an emergency department (ED) urgently for evaluation, as expedited imaging, laboratory tests, and evaluation by a surgeon are critical to early diagnosis and intervention.
- Patients who demonstrate signs of shock should be volume resuscitated and treated with vasopressors as needed.
- Patients with peritoneal signs should have emergent surgical consultation.
- Patients with signs of shock or peritonitis should be treated with intravenous (IV) antibiotics.
- Patients should be treated with analgesics and antiemetics for comfort.
- Patients with clinical concern for acute appendicitis should be kept nil per os (nothing by mouth).
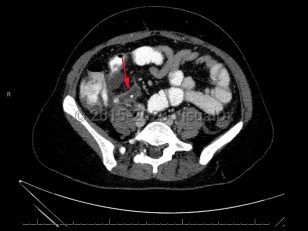
Acute appendicitis is an acute inflammatory condition of the appendix.
Appendicitis results from an obstruction of the appendiceal orifice, which can be caused by a fecalith, lymphoid hyperplasia, infection, calculi, or malignancy. Lymphoid hyperplasia is a more common etiology in younger pediatric patients. Rarely, appendicitis can be caused by infection with the parasitic worm Enterobius vermicularis.
Inflammation begins within the appendiceal lumen and extends through the endothelial wall, leading to focal ischemia, tissue necrosis, and, in some instances, perforation. Perforation can lead to complications including generalized peritonitis and abscess formation.
Acute appendicitis can occur at any age, but it most commonly presents in the second and third decades of life. Lifetime incidence is 8.6% in males and 6.7% in females.
The hallmark symptoms of appendicitis are anorexia, nausea, and emesis, and abdominal pain that radiates or settles in the right lower quadrant (RLQ).
Presentation can vary depending on factors such as patient age and the position of the appendix:
- Neonates – Appendicitis is rare but serious. The most common findings are abdominal distension and/or tenderness, emesis, and poor feeding. Other common findings include lethargy and irritability. There may be delay to diagnosis. Patients may develop sepsis, temperature instability, and dyspnea.
- Infants and toddlers – Appendicitis is infrequent in this population but can occur. The most common findings are abdominal pain (including rebound tenderness and abdominal guarding), fever, and vomiting and anorexia. Diarrhea may occur. The abdomen may or may not be extended. Patients may refuse to walk secondary to pain. Children in this age group are often unable to describe their symptoms or reliably localize their pain.
- School-aged children – Appendicitis is more common than in neonates, infants, and younger children. Abdominal pain (often RLQ), vomiting, anorexia, and fever are common presenting symptoms. Diarrhea is less frequent than in younger children. Patients may have difficulty walking.
- Adolescents – Findings are similar to those of adults with appendicitis.
- Pregnant patients – Appendicitis is the most common nonobstetric surgical emergency in pregnancy and can happen during any trimester, although the second trimester is most common. Typical examination findings may not be present, as guarding and rebound tenderness may be less apparent. It can be more difficult to distinguish uterine tenderness and round ligament pain from appendicular pain in gravid patients. Pregnant patients experience a physiologic leukocytosis, which can also be a challenge in evaluating for appendicitis. Unperforated appendicitis is associated with 3%-5% fetal mortality, but this increases significantly with perforated appendicitis, with 20%-36% fetal mortality,
- Elderly patients – Appendicitis is less common in the elderly, but those older than 65 years still account for roughly 10% of appendicitis cases. In comparison with younger adults, they are more likely to present with atypical or vague symptoms. They are less likely to localize pain to the RLQ. They are more likely to experience complications such as perforation, have increased, albeit still infrequent, mortality, and have increased hospital length of stay.