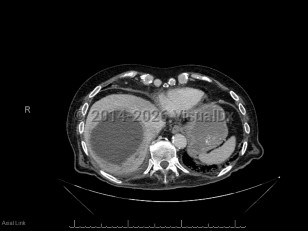
Pyogenic liver abscess
Alerts and Notices
Important News & Links
Synopsis

A pyogenic liver abscess is a collection of pus in the liver as the result of bacterial (or rarely fungal) infection.
The two most common routes that pathogens use to invade the liver and cause an abscess are through the biliary tree (if the biliary tree is obstructed, then cholangitis may follow, which can be complicated by hepatic abscess formation) and through the portal venous system (the portal venous system provides drainage of intraabdominal organs, and pathogens causing diverticulitis or appendicitis, for example, will drain through the portal venous system and may form hepatic abscesses). Liver abscesses may also form due to hematogenous seeding of the liver in the setting of bacteremia. Other intraabdominal abscesses may enlarge and involve the liver by contiguous spread. Rarely, pathogens may seed the liver in the setting of anatomic abnormalities (eg, in the setting of a liver hematoma) or due to direct inoculation in the setting of trauma. In 20%-40% of cases, no obvious cause for the liver abscess is identified.
Many organisms can cause a pyogenic liver abscess, and many abscesses are polymicrobial. Common pathogens include Escherichia coli and Klebsiella species (including the hypermucoid strains of Klebsiella pneumoniae that are a major cause of liver abscess in Asia). Anaerobic organisms are frequently involved, and gram-positive organisms including Streptococcus species and Staphylococcus aureus can also cause abscesses. Candida species may also be involved. Clostridium perfringens liver abscesses can cause hemolysis.
The symptoms of pyogenic liver abscess are nonspecific. The two most common symptoms are fever and abdominal pain. In one review, patients had symptoms for a median of 14 days (range 1-90 days) prior to hospital admission. Some patients will have associated nausea, night sweats, and weight loss. A minority of patients have jaundice. Laboratory evaluation will usually reveal abnormal liver enzymes and an elevated white blood cell count.
Patients with underlying malignancy, cirrhosis, diabetes mellitus, or abnormalities of the pancreas, liver (including liver transplant), or biliary tree are at increased risk of this infection.
Related topic: Amebic Liver Abscess
The two most common routes that pathogens use to invade the liver and cause an abscess are through the biliary tree (if the biliary tree is obstructed, then cholangitis may follow, which can be complicated by hepatic abscess formation) and through the portal venous system (the portal venous system provides drainage of intraabdominal organs, and pathogens causing diverticulitis or appendicitis, for example, will drain through the portal venous system and may form hepatic abscesses). Liver abscesses may also form due to hematogenous seeding of the liver in the setting of bacteremia. Other intraabdominal abscesses may enlarge and involve the liver by contiguous spread. Rarely, pathogens may seed the liver in the setting of anatomic abnormalities (eg, in the setting of a liver hematoma) or due to direct inoculation in the setting of trauma. In 20%-40% of cases, no obvious cause for the liver abscess is identified.
Many organisms can cause a pyogenic liver abscess, and many abscesses are polymicrobial. Common pathogens include Escherichia coli and Klebsiella species (including the hypermucoid strains of Klebsiella pneumoniae that are a major cause of liver abscess in Asia). Anaerobic organisms are frequently involved, and gram-positive organisms including Streptococcus species and Staphylococcus aureus can also cause abscesses. Candida species may also be involved. Clostridium perfringens liver abscesses can cause hemolysis.
The symptoms of pyogenic liver abscess are nonspecific. The two most common symptoms are fever and abdominal pain. In one review, patients had symptoms for a median of 14 days (range 1-90 days) prior to hospital admission. Some patients will have associated nausea, night sweats, and weight loss. A minority of patients have jaundice. Laboratory evaluation will usually reveal abnormal liver enzymes and an elevated white blood cell count.
Patients with underlying malignancy, cirrhosis, diabetes mellitus, or abnormalities of the pancreas, liver (including liver transplant), or biliary tree are at increased risk of this infection.
Related topic: Amebic Liver Abscess
Codes
ICD10CM:
K75.0 – Abscess of liver
SNOMEDCT:
27916005 – Abscess of liver
K75.0 – Abscess of liver
SNOMEDCT:
27916005 – Abscess of liver
Look For
Subscription Required
Diagnostic Pearls
Subscription Required
Differential Diagnosis & Pitfalls

To perform a comparison, select diagnoses from the classic differential
Subscription Required
Best Tests
Subscription Required
Management Pearls
Subscription Required
Therapy
Subscription Required
References
Subscription Required
Last Updated:12/11/2018
Pyogenic liver abscess